- Ischaemic heart disease – 1 year ago
- Occluded LAD with no viability on cardiac MRI
- PCI to proximal LCx
- Heart failure with reduced ejection fraction of 30%
- Primary prevention ICD
- Severe ischaemic secondary mitral regurgitation
- Hyperlipidaemia
- Occasional ex-smoker
- Socially drank alcohol in past, now abstinent
- 57.1 Kg
- 171 cm
- Aspirin 75 mg OD
- Atorvastatin 80 mg OD
- Bisoprolol 2.5 mg OD
- Dapagliflozin 10 mg OD
- Eplerenone 25 mg OD
- Sacubitril/Valsartan 24/26 mg BD
- Furosemide 40 mg BD
- Severely dilated LV with EF: 17%
- Dilated RV
- Severe MR, moderate TR
- PSAP: 71 mm Hg
- Severely dilated LV, LVEF: 29%, LVOT VTI: 6.5 cm, LVIDd I: 4.52 cm/m2, LVIDs I 3.89 cm/m2, LVEDV I: 135.1 ml/m2
- Severely dilated LA
- Dilated RV. TAPSE: 1.49 cm
- Severely dilated RA
- Severe MR, EROA: 0.38cm2
- Moderate TR.
A male in his mid-30s, with BMI of 19.5 kg/m2, and three heart failure hospitalisations in last six months, presented with one month history of gradually worsening shortness of breath on exertion and bilateral leg oedema.
His past medical history included:
Social:
Weight:
Height:
Medications:
Our patient was taking following medications prior to admission:
He had no known drug allergies
On examination patient’s blood pressure was 92/60 mm Hg, heart rate was 88 beats per minute, chest was clear with no crepitations, jugular venous pressure of 14 cm, normal heart sounds with a pan-systolic murmur and bilateral leg oedema till just below knees. He did not have hepatomegaly or ascites.
Investigations on admission:
Haemoglobin: 133 g/L
White blood cell count: 7.1 x 109/L
Platelets: 204 x 109/L
Creatinine: 83 µmole/L
Alanine aminotransferase: 137 U/L
Alkaline phosphatase: 188 U/L
Total bilirubin: 17 µmole/L
NT-ProBNP: 5274 ng/L
ECG: Sinus rhythm at 87 beats/min, P-mitrale, narrow QRS with right bundle branch block morphology, with Q waves in I, aVL, V6.
Chest X-Ray: Clear well inflated lungs.
Based on presentation, patient was diagnosed with acute decompensation of advanced heart failure NYHA (New York heart association) class IV and treatment with intravenous furosemide 80 mg BD was started.
Transthoracic echocardiogram (TTE) on admission:
Repeat TTE 10 days after admission:
| Right heart catheterisation result | ||
|---|---|---|
| Baseline | 10-minutes after starting milrinone infusion at 5 mcg/kg/min | |
| BP (non-invasive, mm Hg) | 80/51 MAP: 61 | 95/58 MAP: 71 |
| RA pressure (mm Hg) | 11 | 6 |
| RV pressure (mm Hg) | 56/9 EDP: 10 | 34/4 EDP: 8 |
| PA pressure (mm Hg) | 57/33 Mean: 42 | 32/19 Mean: 24 |
| PCWP (mm Hg) | 27 | 14 |
| TPG (mm Hg) | 15 | 10 |
| Cardiac output Fick's (L/min) | 2.84 | 5.01 |
| Cardiac index (L/min/m2) | 1.86 | 1.99 |
| PVR (Wood units) | 5.28 | 1.99 |
| SVR (dynes/sec/cm5) | 1408 | 1021 |
| Cardiopulmonary exercise test | |
|---|---|
| Peak VO2 | 18.6 ml/Kg/min (39% of predicted) |
| VE/VCO2 slope | 35 |
| RER: | 1.19 |
| Anaerobic threshold | 12.9 ml/Kg/min |
- NYHA class IV
- Left ventricular ejection fraction (LVEF) <30%, High NT-ProBNP
- Requiring high doses of IV diuretics
- pVO2 <50% predicted
- New York Heart Association (NYHA) classes III and IV or persistently high natriuretic peptide levels
- Left ventricular ejection fraction (LVEF) below 20%
- >1 heart failure hospitalisation in the last year
- Persisting fluid overload (oedema) or increasing diuretic requirement (escalating diuretics)
- Consistently low blood pressure (systolic blood pressure, <90–100 mm Hg)
- Inability to up-titrate or need to reduce/discontinue prognostic medications
- Able to walk 12,000 steps/day
- Able to lie flat
- Minimal leg oedema
- NYHA I-II
- No heart failure admission since discharge
- NT-Pro BNP: 515 ng/L
- Bisoprolol 2.5 mg OD
- Sacubitril/valsartan 97/103 mg BD
- Eplerenone 50 mg OD
- Dapagliflozin 10 mg OD
Our patient was diagnosed with advanced heart failure as he met following criteria from ESC guidelines for the diagnosis of advanced heart failure1:
He also had following markers of poor prognosis from ‘I NEED HELP’ criteria2, in addition to above mentioned advanced heart failure criteria, with an estimated 1-year all-cause mortality of 46.5%3:
In view of advanced heart failure with severe mitral regurgitation, patient was discussed in heart team comprised of advanced heart failure and transplant physicians, interventional cardiologists, cardiac imaging physician and cardio-thoracic surgeons.
Outcome of the meeting was to proceed with mitral transcatheter edge-to-edge repair (TEER) with bridge-to-decision (BTD) intention i.e to improve haemodynamic profile and re-assess for cardiac transplant.
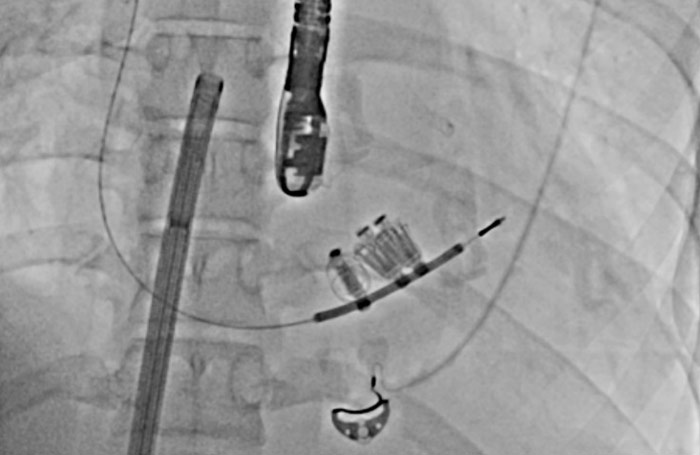
Patient underwent mitral-transcatheter edge-to-edge repair procedure:
Primary access was gained through right femoral vein.
One PASCAL 10 mm clip (Edwards lifesciences LTD) was deployed at A3-P3 and two PASCAL ACE clips (Edwards lifesciences LTD) were deployed at A2-P2.
No major post-procedural complications occurred in our patient and he was started on clopidogrel 75 mg OD, in addition to his usual aspirin, for 3 months.
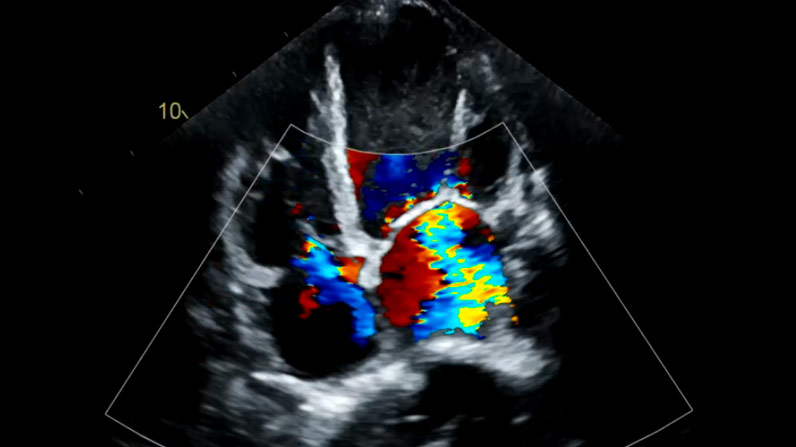
Figure 2: TOE bicommissural view pre-TERR (A) and post TEER (B). Mitral clips can be seen in (B) on the left side. Decrease in size of MR colour jet can be appreciated in (B) compared to (A).
| Right heart catheterisation result | ||
|---|---|---|
| Pre-TEER | 14 day Post TEER | |
| BP (non-invasive, mm Hg) | 80/51 MAP: 61 | 83/54 MAP: 63 |
| RA pressure (mm Hg) | 11 | 18 |
| RV pressure (mm Hg) | 56/9 EDP: 10 | 39/9 EDP: 21 |
| PA pressure (mm Hg) | 57/33 Mean: 42 | 41/24 Mean: 31 |
| PCWP (mm Hg) | 27 | 20 |
| TPG (mm Hg) | 15 | 11 |
| Cardiac output Fick's (L/min) | 2.84 | 3.58 |
| Cardiac index (L/min/m2) | 1.86 | 2.24 |
| PVR (Wood units) | 5.28 | 3.07 |
| SVR (dynes/sec/cm5) | 1408 | 1005 |
| Echocardiography results | ||
|---|---|---|
| Baseline pre-TEER | 7-day Post TEER | |
| MR severity | Severe | Moderate+ |
| MR ERO (cm2) | 0.38 | 0.3 |
| LV EF (%) | 29 | 25-30 |
| LVOT VTI (cm) | 6.5 | 8.4 |
| Cardiopulmonary exercise test result | ||
|---|---|---|
| Baseline pre-TEER | 16-day Post TEER | |
| Peak VO2 (mL/Kg/Min) | 18.6 | 27.4 |
| VE/VCO2 slope | 35 | 23.72 |
Our patient was discharged 15 days after TEER procedure.
Patient profile on 3-month follow-up:
Clinical picture
Blood results
GDMT
Tolerating following regimen:
- Recognition of advanced heart failure according to ESC guidelines1.
- ‘I NEED HELP’ is a useful mnemonic to identify markers of advanced heart failure and refer the patient to advanced heart failure team2.
- Patients with advanced heart failure and secondary severe mitral regurgitation who fulfill COAPT criteria should be considered for TEER. TEER can help delay the need for advanced heart failure therapies (LVAD or transplant) in 22.5% of patients.6
- COAPT criteria includes:
- Secondary MR with severity 3+ or 4+
- NYHA II, III, IV-a
- LV EF ≥20% and ≤50%
- LVIDs ≤70 mm
- Heartmate 3 LVAD therapy is associated with an improved survival and quality of life in advanced heart failure with a median survival beyond 5 years.8
- Heart transplant is not a panacea for advanced heart failure. Heart transplant patients have a median survival of approximately 12 years9. Due to limited donor availability all patients eligible for heart transplant should be refractory to medical therapy.
- LVEF ≤ 30%
- Isolated RV failure
- Non-operable severe valve abnormality
- Non-operable severe congenital abnormality
- Persistently high (or increasing) BNP or NT-ProBNP values and severe LV diastolic dysfunction (according to the definition of HFpEF)
| To diagnose advanced heart failure according to ESC guidelines, all the following criteria must be present despite GDMT: |
|---|
| 1. Severe and persistent symptoms of heart failure (NYHA ≥ 3) |
2. Severe cardiac dysfunction defined by at least one of the following: |
| 3. Episodes of pulmonary or systemic congestion requiring high-dose IV diuretics or episodes of low cardiac output requiring inotropes/vasopressors or malignant arrhythmia causing > 1 unplanned hospitalisation in last 12 months |
| 4. Severely impaired exercise capacity or 6-minute walk test distance <300 m or pVO2 < 12mL/kg/min or <50% predicted value, estimated to be of cardiac origin |
Summary | ||||
|---|---|---|---|---|
| TEER | Surgical mitral valve replacement | Durable LVAD | Cardiac transplant | |
| Benefits | . Minimally invasive . 89.5% procedural success6 . Bailout with surgical replacement possible | . Can delay transplant . Survival rate of 58.4% at 5 years8 | . Option of last resort | |
| Risks | . May not be beneficial if in-appropriately selected patients10 | . Invasive procedure . TEER non-inferior to surgical mitral valve repair/replacement7 . Peri-procedural morbidity/mortality can be calculated using STS score | . 2.1% device thrombosis8 . 10.7% stroke8 . 45.8% bleeding risk8 . 22.7% drive line infection8 | . Median survival of 12 years9 |
| Availability | No waiting time | No waiting time | No waiting time | Waiting list |
- McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Böhm M, et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: Developed by the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) With the special contribution of the Heart Failure Association (HFA) of the ESC. European Heart Journal. 2021;42(36):3599-726.
- Pagnesi M, Ghiraldin D, Vizzardi E, Chiarito M, Stolfo D, Baldetti L, et al. Detailed Assessment of the “I Need Help” Criteria in Patients With Heart Failure: Insights From the HELP-HF Registry. Circulation: Heart Failure. 2023;16(12):e011003.
- Pagnesi M, Lombardi CM, Chiarito M, Stolfo D, Baldetti L, Loiacono F, et al. Prognostic impact of the updated 2018 HFA-ESC definition of advanced heart failure: results from the HELP-HF registry. Eur J Heart Fail. 2022;24(9):1493-503.
- Vahanian A, Beyersdorf F, Praz F, Milojevic M, Baldus S, Bauersachs J, et al. 2021 ESC/EACTS Guidelines for the management of valvular heart disease: Developed by the Task Force for the management of valvular heart disease of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). European Heart Journal. 2021;43(7):561-632.
- Stone GW, Lindenfeld J, Abraham WT, Kar S, Lim DS, Mishell JM, et al. Transcatheter Mitral-Valve Repair in Patients with Heart Failure. New England Journal of Medicine. 2018;379(24):2307-18.
- Marcelli C, Munafo' AR, Estevez-Loureiro R, Adamo M, Guerin P, Arzamendi D, et al. Transcatheter edge to edge repair of functional mitral regurgitation as bridge to heart transplantation: 2-years follow up results from MitraBridge international registry. European Heart Journal. 2023;44(Supplement_2).
- Baldus S, Doenst T, Pfister R, Gummert J, Kessler M, Boekstegers P, et al. Transcatheter Repair versus Mitral-Valve Surgery for Secondary Mitral Regurgitation. New England Journal of Medicine. 2024;391(19):1787-98.
- Mehra MR, Goldstein DJ, Cleveland JC, Cowger JA, Hall S, Salerno CT, et al. Five-Year Outcomes in Patients With Fully Magnetically Levitated vs Axial-Flow Left Ventricular Assist Devices in the MOMENTUM 3 Randomized Trial. JAMA. 2022;328(12):1233-42.
- Khush KK, Cherikh WS, Chambers DC, Goldfarb S, Hayes D, Jr., Kucheryavaya AY, et al. The International Thoracic Organ Transplant Registry of the International Society for Heart and Lung Transplantation: Thirty-fifth Adult Heart Transplantation Report—2018; Focus Theme: Multiorgan Transplantation. The Journal of Heart and Lung Transplantation. 2018;37(10):1155-68.
- Obadia J-F, Messika-Zeitoun D, Leurent G, Iung B, Bonnet G, Piriou N, et al. Percutaneous Repair or Medical Treatment for Secondary Mitral Regurgitation. New England Journal of Medicine. 2018;379(24):2297-306.
BMI: Body mass index
PCI: Percutaneous coronary intervention
LAD: Left anterior descending coronary artery
LCx: Left circumflex coronary artery
ICD: Implantable cardioverter defibrillator
EF: Ejection fraction
PSAP: Pulmonary artery systolic pressure
LVOT VTI: Left ventricle outflow tract velocity time integral
LVIDd I: Left ventricle internal diameter end-diastole indexed
LVIDs I: Left ventricle internal diameter end-systole indexed
LVEDV I: Left ventricle end-diastolic volume indexed
TAPSE: Tricuspid annular plane systolic excursion
EROA: Effective regurgitant orifice area
EDP: End diastolic pressure
PCWP: Pulmonary capillary wedge pressure
TPG: Transpulmonary gradient
PVR: Pulmonary vascular resistance
SVR: Systemic vascular resistance
RER: Respiratory exchange ratio
GDMT: Guideline directed medical therapy
Disclaimer
This case report and/or content does not reflect the opinion of iHF or iheartfunction.com, nor does it engage their responsibility.