- Non-smoker
- No alcohol consumption
- Blood pressure: 92/61 mmHg
- Heart rate: 101
- Cardiac auscultation revealed S1, S2 heart sounds with S3 and a holosystolic murmur by left parasternal border.
- Bilateral pretibial edema was present (+3).
- BNP:4500 pg/ml, creatinine:1.3 mg/dl, potassium:4.8 pg/ml
- ECG: 2nd day Electrocardiogram demonstrated sinus rhythm (SR) with a heart rate (HR) of 82 beats per minute with signs of atrial dilatation.
- Chest CT: Thoracic computed tomography (CT) revealed an increased cardiothoracic ratio. The pulmonary trunk diameter was enlarged at 35 mm. The trachea and main bronchi were patent. There was an increase in the amount of pleural effusion on the left hemithorax, measuring approximately 2 cm. Interlobular septal thickening was noted bilaterally. Additionally, peripheral predominant ground-glass opacities and consolidations were observed in the right lung, consistent with the findings on the patient’s previous imaging.
- Left ventricular ejection fraction (LVEF): 15% (global hypokinesia with spontaneous echo contrast within left ventricle)
- Mitral regurgitation: Moderate (EROA 0.19 cm²)
- Tricuspid regurgitation: Severe (grade 3)
- Systolic pulmonary artery pressure: 50–55 mmHg
- No regional wall motion abnormalities observed in the left ventricle
- Hepatic veins and inferior vena cava (IVC) diameter 2.1 cm with reduced respiratory collapse
- Left atrium diameter: 5.5 mm
- Lead from ICD appropriately positioned in the dilated right heart structures
- New York Heart Association (NYHA) Class III symptoms
- LVEF <30%
- Elevated NT-proBNP levels
- Requirement for high-dose intravenous diuretics
- NYHA Class III symptoms
- LVEF below 20%
- More than one heart failure hospitalization within the last year
- Persistent fluid overload and escalating diuretic requirement
- Persistent low systolic blood pressure (<90–100 mmHg)
- Inability to tolerate or uptitrate guideline-directed medical therapy
A 36-year-old male patient who had been diagnosed as Becker muscular dystrophy (BMD) 25 years ago, presented with acute decompensated heart failure (ADHF), having had three hospitalizations in the last three months requiring high doses of diuretics. The patient reported a one-month history of progressively worsening exertional dyspnea and bilateral lower extremity edema.
Medical history
The patient’s past medical history was notable for Becker muscular dystrophy along with compatible physical findings, i.e, significant proximal muscle atrophy and calf pseudohypertrophy. Hence, he was bound by a wheelchair.
He also suffered from deep vein thrombosis, and pulmonary thromboembolism in 2018 in relation to immobility.
He was diagnosed to have heart failure in 2006 and underwent primary prophylaxis with a St. Jude implantable cardioverter-defibrillator (ICD-VVI) in 2016.
There is no history of coronary artery disease.
History was remarkable for several on and off in relation to HF medications along with low adherence due to low blood pressure, which has become more apparent in recent years.
Cardiac status
Echocardiographic findings were consistent with heart failure with reduced ejection fraction (HFrEF), characterized by a dilated left ventricle.
Social history
Investigation on admission
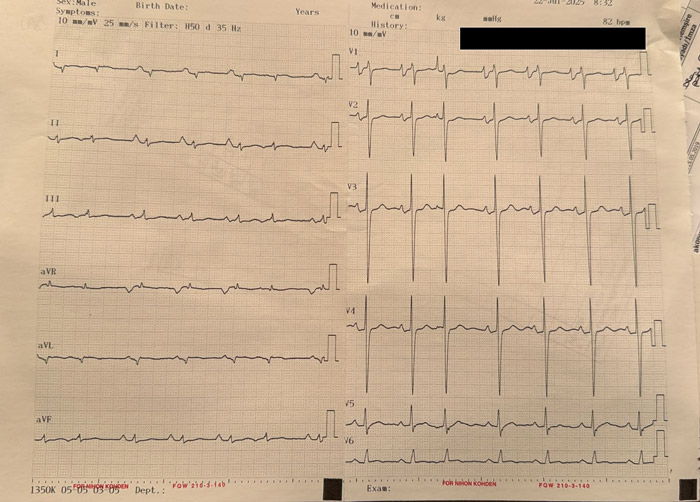
12-lead ECG of the patient at admission
Transthoracic echocardiography (TTE)
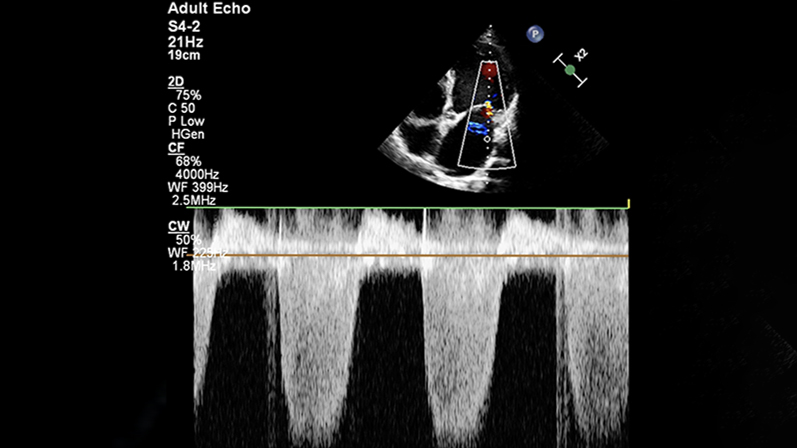
Echocardiography wtih 4-chamber view and continuous Doppler at mitral valve
Video of 4-chamber view echocardiography
Clinical Assessment
The patient, along with his history in the last year is consistent with the European Society of Cardiology (ESC) 2021 guidelines criteria for advanced heart failure, including:
Additionally, the patient met several markers of poor prognosis defined by the AHA’s 'I NEED HELP' criteria1, associated with an estimated one-year all-cause mortality rate of approximately 46.5%:
- Ivabradine 5 mg twice Daily: 8 a.m, 8 p.m (1st day)
- Digoxin 0.125 mg once Daily: 8 a.m (1st day, 5 times/week)
- Empagliflozin 10 mg once Daily: 11 a.m (2nd day)
- Spironolactone 25 mg once Daily: 2 p.m (3rd day)
- Switch to Sacubitril/valsartan 24/26 mg twice Daily: 8 a.m, 8 p.m (5th day with the first dose at the evening)
Management and Decision-Making
The patient’s medical therapy for heart failure with reduced ejection fraction (HFrEF) has been optimized thoroughly along with succesful decongestion via intravenous infusion of furosemide at 5-10 mg/hour dose for 6 days. The patient was on low dose ARB before admission with no tolerance to beta blockers previously. He was on strict low salt diet.
Despite persistent low blood pressure with fluctuating hypotensive symptoms during the course of hospitalization, “start low go slow principle” has been implemented and doses were carefully adjusted according to the peak effect of each agent.
As initial plan, low salt diet was abandoned and in order to control sinus tachycardia, ivabradine 5 mg was administered bid given that resting heart rate is elevated in the absence of significant secondary reason given that the patient was intolerant to beta blockers1.
Additionally, digoxin was added for heart rate control (1) to decrease further HF related hospitalization.
The medical regimen was initiated as follow:
Of note, he was completely intolerant to each trial of different beta blockers. The patient was also anticoagulated parenterally during hospitalization not only related to spontaneous echo contrast within the heart but also to history of deep vein thrombsis and pulmonary embolism and then switched to apixaban 5 mg twice Daily: 10 a.m, 10 p.m (before discharge).
Lab at discharge: BNP:1100 pg/ml, creatinine:1.2 mg/dl, potassium:4.9 pg/ml
Furthermore, the patient was referred to the inpatient respiratory and mobilization physiotherapy program in order to improve muscle weakness and low peripheral vascular resistance.
Given the history of frequent hospitalization with intolerance to optimal medical therapy, the patient, who had an INTERMACS profile of 4, was evaluated for left ventricular assist device (LVAD) implantation. Neurology consultance was obtained and it yielded moderate to high perioperative neurological risk. Special precautions were advised regarding malignant hyperthermia susceptibility during anesthesia. The patient and his family are currently discussing the options. He was discharged from the hospital with an outpatient appointment at the 10th day. A very low dose selective beta blocker is planned at the first visit along with outpatient hospitalization.
Literature reports demonstrate successful outcomes of LVAD implantation and heart transplantation in selected patients with Becker muscular dystrophy2. Critical factors influencing candidacy and postoperative prognosis include preserved respiratory function, adequate mobility, and swallowing capacity.
Specific cardiomyopathies which yield HFrEF phenotype are treated as such via quadruple GDMT though these patients are usually excluded from the clinical trials in which evidence is generated.
In these patients, several problems can potentially interfere with optimization of GDMT, and low blood pressure is a critical limiting factor.
However, as pointed out in the recent consensus statement of HFA3, it is possible to achieve much of the GDMT, and herein, SGLT2 inhibitors and MRA are potentially the most straightforward agents to begin with.
- Theresa A McDonagh, Marco Metra, Marianna Adamo, Roy S Gardner, Andreas Baumbach, Michael Böhm, Haran Burri, Javed Butler, Jelena Čelutkienė, Ovidiu Chioncel, John G F Cleland, Andrew J S Coats, Maria G Crespo-Leiro, Dimitrios Farmakis, Martine Gilard, Stephane Heymans, Arno W Hoes, Tiny Jaarsma, Ewa A Jankowska, Mitja Lainscak, Carolyn S P Lam, Alexander R Lyon, John J V McMurray, Alexandre Mebazaa, Richard Mindham, Claudio Muneretto, Massimo Francesco Piepoli, Susanna Price, Giuseppe M C Rosano, Frank Ruschitzka, Anne Kathrine Skibelund, ESC Scientific Document Group , 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: Developed by the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) With the special contribution of the Heart Failure Association (HFA) of the ESC, European Heart Journal, Volume 42, Issue 36, 21 September 2021, Pages 3599–3726, https://doi.org/10.1093/eurheartj/ehab368
- Gyoten T, Amiya E, Kinoshita O, Tsuji M, Kimura M, Hatano M, Ono M. Clinical outcomes of continuous flow left ventricular assist device therapy as bridge to transplant strategy in muscular dystrophy: a single-center study. Gen Thorac Cardiovasc Surg. 2023 Jun;71(6):347-353. doi: 10.1007/s11748-022-01889-1. Epub 2022 Nov 8. PMID: 36348232.
- Skouri H, Girerd N, Monzo L, Petrie MC, Böhm M, Adamo M, Mullens W, Savarese G, Yilmaz MB, Amir O, Bayes-Genis A, Bozkurt B, Butler J, Chioncel O, Mebazaa A, Merino JL, Moura B, Ponikowski P, Seferovic P, Rosano GMC, Metra M. Clinical management and therapeutic optimization of patients with heart failure with reduced ejection fraction and low blood pressure. A clinical consensus statement of the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail. 2025 Apr;27(4):707-722. doi: 10.1002/ejhf.3618.
- Mustafa Goktug Erata: None
- Mehmet Birhan Yilmaz: has received institutional fee from Bayer, Amgen, Novartis, Astra Zeneca, Boehringer Ingelheim, Novo Nordisk, Albert Health
Disclaimer
This case report and/or content does not reflect the opinion of iHF or iheartfunction.com, nor does it engage their responsibility.




